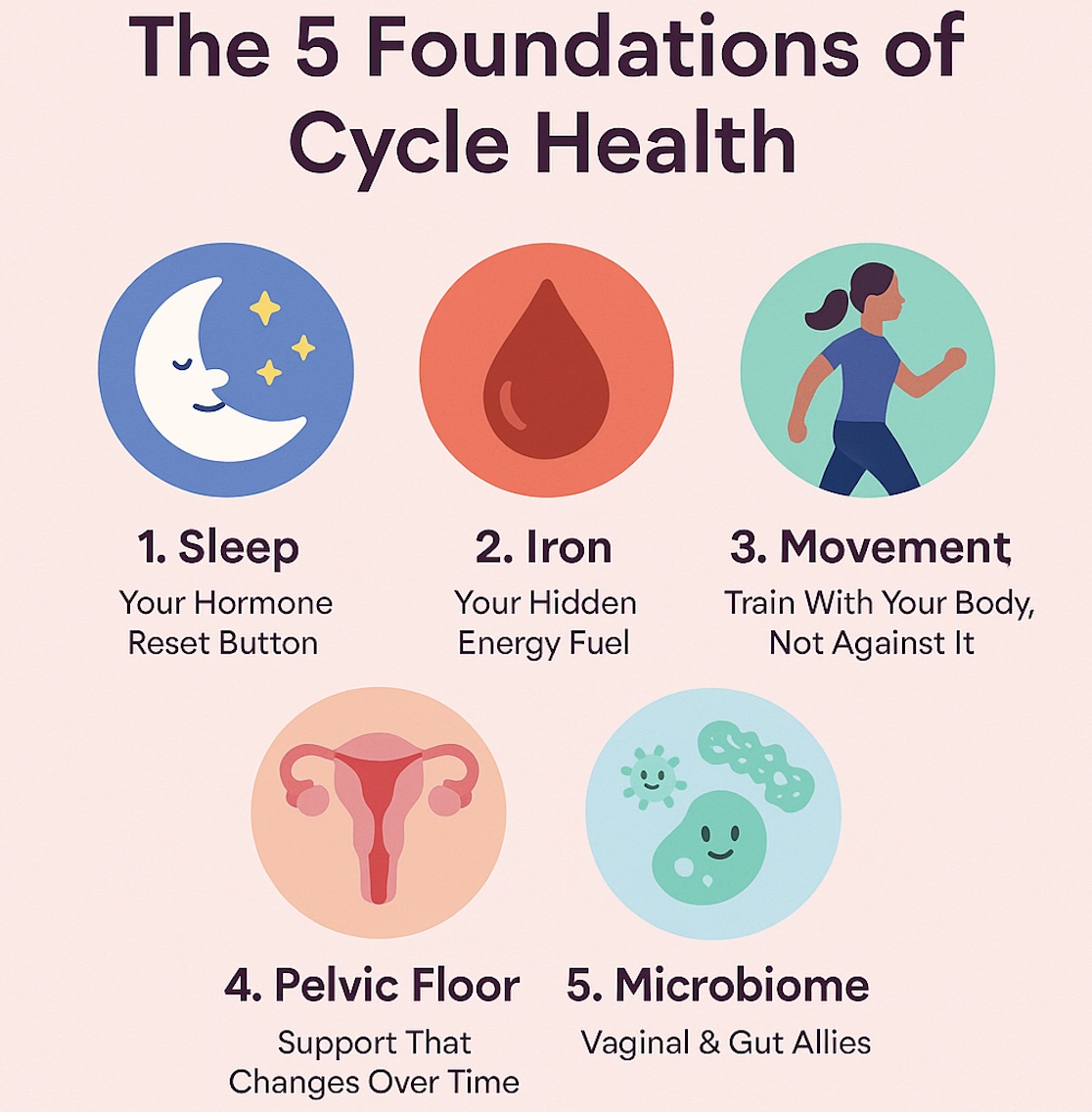
Why this matters: No matter your age or stage, first periods, postpartum, perimenopause, or post-menopause: five basics consistently shape how you feel across the month:
- sleep
- iron status
- movement
- pelvic floor health
- and your microbiome
Mastering these pillars helps with energy, mood, focus, cramps, bladder comfort, and long-term well-being. Below is a practical, evidence-aware guide with simple actions you can start today and track in Life.
1) Sleep: Your Hormone Reset Button
Hormones and sleep talk to each other all month long. Fluctuations in the cycle can nudge sleep quality, and in turn, irregular sleep can lengthen cycles and worsen PMS for some people. Recent research links later sleep timing and “social jetlag” with more disrupted cycle rhythms; elite-athlete data also show cycle phase and symptom burden can influence sleep and recovery.
Do this now
-
Anchor your wake-up time (even on weekends). Stability beats perfection for circadian health.
-
Create a wind-down: dim lights, warm shower, and screens off 60 minutes before bed.
-
In Life, log sleep quality for a week. Notice patterns vs. phases (bleeding days, mid-cycle, late luteal). If you see a late-luteal dip, try an earlier bedtime by 30–45 minutes for those days.
When to get help: Loud snoring, breath pauses, persistent insomnia, or severe daytime sleepiness warrant medical evaluation (sleep apnea and insomnia are treatable).
2) Iron: Energy, Focus, and Hair Health
If you bleed, you lose iron: period. Adolescents, heavy-bleeders, athletes, and perimenopausal users are especially at risk of iron deficiency (ID) and iron-deficiency anemia (IDA), which can show up as fatigue, brain fog, hair shedding, brittle nails, or shortness of breath. Public-health guidance has long recommended periodic screening for ID/IDA in non-pregnant females, and newer discussions emphasize how common it is in teens.
Do this now
-
If you log heavy flow (e.g., changing a super pad/tampon every 1–2 hours for several hours, or bleeding >7 days), ask your clinician about a CBC and ferritin.
-
Pair plant iron (beans, lentils, spinach) with vitamin C (citrus, peppers) to boost absorption.
-
If you supplement, do it with medical advice: dose and duration depend on your labs.
-
In Life, turn on Heavy Flow and Symptoms (fatigue, dizziness, headaches) to spot trends and share screenshots at appointments.
3) Movement: Train With Your Body, Not Against It
“Cycle syncing” (tailoring workouts by phase) is everywhere online. The idea is appealing, but experts caution that evidence is still emerging and claims about guaranteed productivity or huge fitness gains are overstated. What we do know from real-world data (including Apple Women’s Health Study updates) is that activity can vary by bleeding vs. non-bleeding days, and listening to symptoms is smart. The safest, most evidence-aligned approach: flexible, symptom-aware training that adapts volume and intensity to how you feel, without rigid rules.
Do this now
-
Build a minimum-dose routine you can keep on low-energy days: 10–20 minutes of walking, mobility, or light strength.
-
On better-energy days, progress load: intervals, lifting, or longer sessions.
-
Track in Life: rate Energy, Cramps, Mood, and Workout Type. After 1–2 cycles, you’ll see your personal response patterns, more useful than generic calendars.
Teens & beginners: Focus on movement skill (form, balance, coordination) and consistency.
Perimenopause & menopause: Prioritize resistance training (2–3x/week) and impact (as tolerated) for muscle, bone, and metabolic health.
4) Pelvic Floor: Support That Changes Over Time
Pelvic floor disorders (leakage, urgency, heaviness/prolapse) affect a quarter or more of women, with risk shaped by pregnancy, birth, time, and hormones. A lifespan perspective shows “functional reserve” is highest early on and changes with milestones like childbirth and menopause: so proactive care pays off.
Do this now
-
Learn “the basics”: your pelvic floor should contract, relax, and lengthen. Constant clenching can be as problematic as weakness.
-
Adopt the “brace-exhale-move” habit for lifts and cough/sneeze moments.
-
If you have leakage, pelvic pain, pressure, or recurrent urgency, a pelvic floor physio can individualize strategies (not everyone needs Kegels; some need down-training and breath work).
-
In Life, add a Pelvic Health custom tag to log triggers (long runs, heavy lifts, late-luteal bloating).
5) Microbiome: Vaginal & Gut Allies
The vaginal microbiome (especially Lactobacillus species) helps maintain a healthy, low-pH environment. Growing evidence suggests targeted probiotics may support recurrent bacterial vaginosis (BV) or vulvovaginal candidiasis (yeast) for some users, and research is exploring links with conditions like endometriosis and adenomyosis. Results vary by strain and product quality. Think of probiotics as an adjunct, not a cure-all.
Do this now
-
Support the ecosystem: avoid over-washing and harsh soaps; use breathable underwear; change out of sweaty clothes soon after workouts.
-
If you face recurrent BV/yeast, talk to your clinician about evidence-based strains and timing relative to standard treatment.
-
Track discharge, itch, odor, and antibiotic use in Life to spot patterns and share at visits.
A Note on GLP-1 Medications (Ozempic/Wegovy and others)
Many users ask how GLP-1 medications interact with cycles and symptoms. Early evidence in populations with PCOS suggests GLP-1 receptor agonists may improve menstrual regularity and ovulation, likely through metabolic benefits, while researchers continue to study endometrial effects and long-term safety. If you’re on these medicines, log bleeding patterns, cramps, and mood to personalize care with your clinician.
When to Seek Care (All Ages)
-
Heavy bleeding (soaking through protection hourly for several hours), cycles <21 or >90 days, new post-menopausal bleeding, or severe pain need evaluation.
-
Persistent fatigue, dizziness, or exercise intolerance: ask about CBC + ferritin.
-
Recurrent BV/yeast or persistent discharge/odor changes, get tested and discuss targeted care.
-
Pelvic pressure, bladder leakage, or pain: a pelvic floor physio plus clinician can help.
-
Sleep disorders or loud snoring: consider a sleep evaluation.
Trends come and go (hello, cycle syncing), but the foundations rarely change. If you steadily improve sleep, protect iron, move with flexibility, care for your pelvic floor, and support your microbiome and track what actually helps you, you’ll feel the difference at 15, 35, or 55. Use Life to turn these into tiny weekly commitments, measure how you feel, and build your own evidence.
Info References
-
Cycle-phase, sleep & performance: recent studies on sleep/cycle timing and elite athletes’ recovery. SpringerLink+1
-
Cycle syncing claims vs. evidence. BMJ+1
-
Iron deficiency & screening in menstruating users and adolescents. jamanetwork.com+2PMC+2
-
Pelvic floor across the lifespan; guideline perspectives. PMC+1
-
Vaginal microbiome & probiotic evidence; emerging links to gynecologic conditions. Frontiers+3PMC+3MDPI+3
-
GLP-1 medications and cycles/PCOS; ongoing endometrial research. Bioscientifica+2PMC+2
Medical Disclaimer
This article is for informational purposes only and should not replace professional medical advice. Always consult your healthcare provider before making significant dietary changes, especially if you have a medical condition or are on medication.